October is Menopause Awareness Month, and it’s an especially important time for us at Yowwig to shed light on the unique challenges faced by young women who have been affected by gynaecological cancers. In some young women, cancer treatments have resulted in menopause for example, surgical menopause, a life-changing event that can bring both physical and emotional hurdles. While menopause is a natural stage of life, entering menopause earlier than expected, especially due to cancer treatment, requires a different kind of vigilance and care.
Understanding Surgical Menopause
Surgical menopause occurs when a woman’s ovaries are removed as part of cancer treatment, which leads to a sudden drop in hormone levels. Unlike natural menopause, which happens gradually, surgical menopause brings immediate symptoms, often more intense, including hot flushes, mood swings, and vaginal dryness. It’s not just the physical symptoms, many women in their 20s, 30s, and 40s are suddenly thrust into a stage of life they weren’t expecting for decades. This can be emotionally overwhelming and isolating.
At Yowwig, we know that for young women who are battling or have survived gynaecological cancers like ovarian, uterine, and cervical cancer, surgical menopause adds another layer of complexity to your journey. It can feel unfair and daunting, but it’s also a reminder of your incredible strength and resilience.
Menopause Symptoms vs. Gynaecological Cancer Symptoms
One of the key messages this month is the importance of staying vigilant about your health, especially if you’re experiencing surgical menopause. Symptoms such as hot flushes and night sweats may be expected, but if you notice abnormal bleeding, pelvic pain, bloating, or other unusual changes, these could signal more than just menopausal symptoms.
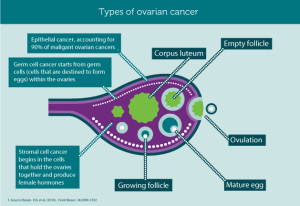
Gynaecological cancers can sometimes mimic the signs of menopause, which is why it’s critical to pay attention to your body and seek medical advice when something feels off. Ovarian, uterine, and cervical cancers are particularly important to monitor during and after menopause. While you may associate menopause with age, cancer-related menopause can complicate things, making it harder to distinguish between what’s “normal” and what needs urgent attention.
Taking Charge of Your Health
One of the most empowering things you can do this Menopause Awareness Month is to take charge of your health. Be proactive—schedule regular check-ups, know the signs and symptoms of gynaecological cancers, and don’t hesitate to raise concerns with your healthcare provider.
Cancer survivors often live with the lingering fear of recurrence, but staying informed and aware can help reduce that fear and keep you in control. Early detection is the key to saving lives, and it’s a reminder that awareness starts with you.
Emotional Support is Key
The emotional toll of going through surgical menopause at a young age can be heavy. Many women feel a loss of femininity, experience anxiety or depression, or struggle with the rapid changes their bodies go through. It’s important to acknowledge these feelings and seek support. Whether it’s through a support group, talking to a therapist, or connecting with other women in the Yowwig community, you don’t have to go through this alone.
We understand that surgical menopause can feel like yet another obstacle, but you are not defined by your cancer or your menopause. You are bold, resilient, and strong—and at Yowwig, we’re here to support you every step of the way.
Join the Conversation
This Menopause Awareness Month, let’s continue the conversation about the intersection of gynaecological cancers and menopause. By sharing your story, you might just help another young woman feel less alone. Together, we can raise awareness, support each other, and push for better understanding and treatment options for those experiencing surgical menopause.
If you or someone you know is dealing with unusual symptoms, please don’t dismiss them as “just menopause.” Talk to your healthcare provider, stay informed, and remember that early detection can make all the difference.
#MenopauseAwarenessMonth #GynaecologicalCancer #SurgicalMenopause #WomensHealth #CancerSurvivor #EarlyDetectionMatters